- En
- Fr
- عربي
The Role of Strategic Planning in Enhancing Health Systems in Fragile States
Introduction
Background and Context
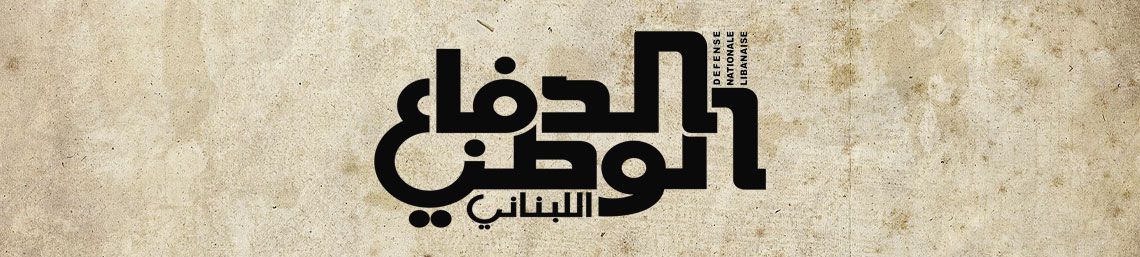
Fragile states are characterized by a lack of strong governance, political instability, and inadequate public services. These states often face chronic instability due to internal conflicts, corruption, economic challenges, and poor infrastructure. The governance in such states is typically weak, resulting in limited capacity to provide basic services, including healthcare, education, and security. The lack of effective institutions and social cohesion exacerbates the fragility, making these states susceptible to various crises1.
There is no universally accepted definition of a 'fragile state'. While there is consensus that some states are fragile, labeling others is more contentious. Further debate surrounds the classification of a fragile state’s status, whether it is declining into fragility, languishing in fragility, or stabilizing after a volatile period. The country's baseline development index, whether it is a middle- or high-income country or a low-income one, along with its geopolitical and strategic position, also influences its impact on the global level2.
In fragile states, robust health systems play a crucial role in maintaining societal stability and development. A well-functioning health system ensures that essential services are available to the population, thereby improving overall health and well-being. Additionally, strong health systems help prevent and control the spread of diseases, which is particularly important in regions prone to outbreaks of infectious diseases. By providing consistent and reliable healthcare, governments can build trust with their citizens, enhancing their legitimacy and fostering social cohesion. This, in turn, can contribute to reducing conflict and promoting peace.
Health systems in fragile states encounter numerous challenges that hinder their effectiveness, including resource constraints such as limited financial resources, inadequate healthcare infrastructure, and shortages of medical supplies and personnel. Political instability, characterized by frequent changes in government, corruption, and weak governance, disrupts healthcare delivery and impedes long-term planning. Conflict and violence further damage healthcare infrastructure, displace populations, and create unsafe conditions for healthcare workers. These states are also highly vulnerable to public health crises, with disease outbreaks quickly overwhelming already strained health systems. Social and cultural barriers, including social inequalities and cultural norms, restrict access to healthcare for certain population groups, leading to disparities in health outcomes. Additionally, fragmented efforts and a lack of coordination among various stakeholders, including government agencies, non-governmental organizations, and international bodies, result in inefficiencies and duplication of efforts.
This essay argues that strategic planning is essential for strengthening health systems in fragile states. By establishing clear goals, priorities, and action plans, strategic planning enhances coordination, resource allocation, and system resilience, ultimately leading to improved healthcare outcomes and greater stability in fragile contexts.
Chapter One
Understanding Fragile States
A. Defining Fragile States
Most definitions of fragile states consider fragility as existing on a spectrum between two extremes: complete state failure and collapse on one end, and states with significant vulnerabilities on the other. These definitions generally agree that fragile states have governments that struggle to ensure basic security, fail to provide essential services and economic opportunities, and lack the legitimacy needed to maintain citizen trust. Citizens in these states are often divided along ethnic, religious, or class lines, with deep-seated histories of distrust, grievances, and violent conflict. This lack of capacity for cooperation, compromise, and trust can push states towards failure, collapse, crisis, and violent conflict. Post-conflict and recovering states must find ways to rebuild capacity, address these deficits, and avoid the constant threat of regression3.
A fragile state typically exhibits several attributes, manifesting in various ways, including the loss of physical control over its territory or a monopoly on the legitimate use of force, the erosion of legitimate authority to make collective decisions, an inability to provide reasonable public services, and the inability to interact with other states as a full member of the international community4.
Fragile states are identified based on a range of political, economic, and social indicators that highlight their vulnerabilities and governance challenges.
Political Indicators: These include the level of political stability, governance quality, rule of law, and corruption. Fragile states often suffer from weak governance structures, lack of effective institutions, political violence, frequent changes in government, and widespread corruption. The inability to enforce laws and provide security undermines the state's legitimacy and capacity to function effectively.
Economic Indicators: Economic fragility is marked by low GDP per capita, high unemployment rates, poor infrastructure, and economic dependence on a narrow range of sectors (often commodities). These states typically face significant economic instability, lack of investment, and minimal economic diversification, which exacerbate poverty and limit growth opportunities.
Social Indicators: Social criteria include health, education, and social cohesion metrics. Fragile states often have low literacy rates, poor health outcomes, and high levels of social inequality and exclusion. The social fabric is typically weakened by ethnic, religious, or regional divisions, which can lead to conflict and further destabilize the state5.
Examples of Fragile States
Examples of fragile states include:
• Afghanistan: Plagued by decades of conflict, political instability, and governance issues, Afghanistan faces severe challenges in governance and service delivery.
• South Sudan: Since gaining independence in 2011, South Sudan has struggled with ongoing civil conflict, political fragmentation, and economic hardship.
• Haiti: Persistent political instability, natural disasters, and economic difficulties have contributed to Haiti's fragility.
• Somalia: Somalia has been marked by decades of civil war, terrorism, and weak central governance, resulting in a fragile state with significant security and development challenges.
B. Health Challenges in Fragile States
Common Health Issues and Disparities
Health systems in fragile states face numerous challenges, leading to poor health outcomes and significant disparities in healthcare access and quality.
• High Burden of Disease: Fragile states often have high rates of infectious diseases such as malaria, tuberculosis, and HIV/AIDS, compounded by poor sanitation and limited access to clean water. Non-communicable diseases (NCDs) are also rising due to changing lifestyles and urbanization.
• Maternal and Child Health: High maternal and child mortality rates are prevalent due to inadequate prenatal and postnatal care, poor nutrition, and lack of skilled birth attendants.
• Limited Healthcare Infrastructure: Health facilities are often under-resourced, understaffed, and poorly maintained, with limited access to essential medicines and medical supplies.
• Health Workforce Shortages: There is a significant shortage of trained healthcare professionals, exacerbated by brain drain, poor working conditions, and inadequate training facilities.
• Inequities in Health Access: Vulnerable groups, including women, children, and marginalized communities, face significant barriers to accessing healthcare services, leading to health disparities.
Impact of Instability and Conflict on Healthcare Delivery
Instability and conflict have profound impacts on healthcare delivery in fragile states:
• Destruction of Health Infrastructure: Conflict and violence often result in the destruction of hospitals, clinics, and other health facilities, further limiting healthcare access.
• Displacement of Populations: Conflict-induced displacement forces people into overcrowded camps with poor living conditions, increasing the risk of disease outbreaks and straining existing health services.
• Disruption of Health Services: Ongoing violence and instability disrupt the delivery of essential health services, including immunization programs, maternal and child health services, and disease prevention efforts.
• Safety of Healthcare Workers: Healthcare workers are frequently targeted or caught in the crossfire during conflicts, leading to a decline in the workforce and reduced availability of services.
• Psychosocial Impact: Prolonged conflict and instability have significant mental health implications, contributing to increased rates of trauma, depression, and anxiety among affected populations.
Understanding the unique challenges faced by health systems in fragile states is crucial for developing effective strategic planning initiatives to enhance healthcare delivery and outcomes.
Chapter Two
Importance of Strategic Planning in Health Systems
A. Definition and Components of Strategic Planning
Definition of Strategic Planning
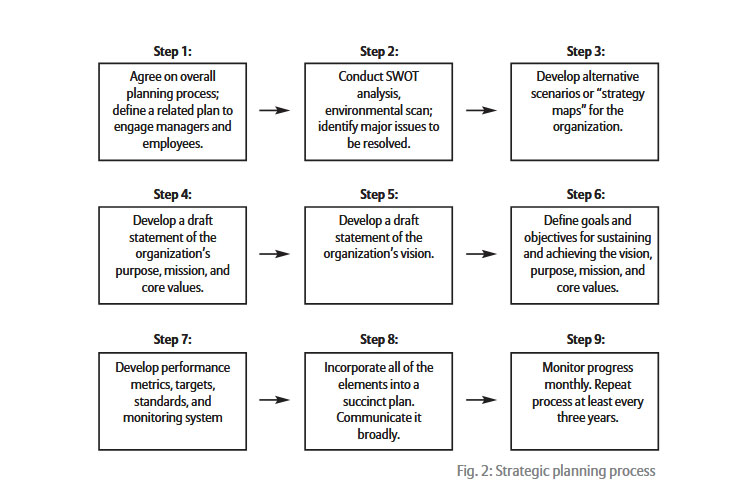
Strategic planning in health systems refers to the process of defining a health system's direction, setting priorities, allocating resources, and implementing actions to achieve specific health goals. It involves a systematic and coordinated approach to addressing health challenges, improving service delivery, and ensuring sustainable health system performance.
Strategic planning in healthcare benefits from a holistic mindset, facilitating the identification and resolution of issues with a patient-focused perspective. Strategists should be able to systematically identify problems using factors such as urgency, impact, and feasibility. This toolkit provides a strategic method for navigating complex healthcare challenges. Urgency helps distinguish between issues requiring immediate action and those suitable for phased resolution. Impact ensures prioritized problems align with organizational goals, driving decisions toward meaningful and sustainable outcomes. Feasibility introduces practicality, grounding strategic plans in reality. In strategic healthcare planning, the initial step is to accurately assess our current position by identifying our strengths, weaknesses, opportunities, and threats. The second step is to clearly define our future objectives. Next, we must analyze the gap between our current position and our goals, resulting in a list of gaps that need to be addressed to achieve our objectives. We should then prioritize these gaps based on their significance. The following step is to develop solutions for each identified gap. Finally, we must rank these solutions by their impact and cost, prioritizing low-cost, high-impact solutions to maximize efficiency and effectiveness6.
Strategic planning in healthcare is vital for three main reasons. Firstly, it helps organizations adapt to the rapidly changing healthcare environment, ensuring they remain relevant and effective. Secondly, it allows for the efficient allocation of limited resources by identifying critical needs and aligning resources with organizational goals. Lastly, strategic planning aids in setting priorities and making informed decisions, enabling healthcare organizations to evaluate options and align actions with their long-term objectives7.
B. Benefits of Strategic Planning
Enhanced Coordination and Resource Allocation
Strategic planning fosters collaboration and coordination among various stakeholders, including government agencies, healthcare providers, non-governmental organizations, and international partners. By aligning efforts and resources, strategic planning ensures a unified approach to addressing health challenges and achieving common goals. Also, Strategic planning enables health systems to prioritize resource allocation based on identified needs and strategic objectives. It helps in directing limited resources to high-impact areas, reducing wastage, and ensuring that funds, personnel, and equipment are used efficiently and effectively.
Improved Healthcare Outcomes and System Resilience
By setting clear objectives and implementing targeted strategies, strategic planning leads to improved health outcomes. It helps in addressing critical health issues, reducing disease burden, and enhancing the quality and accessibility of healthcare services. Strategic planning also facilitates the introduction of evidence-based practices and innovative solutions that contribute to better health results. On the other hand, strategic planning builds the resilience of health systems by preparing them to respond effectively to crises and challenges. It involves assessing risks, developing contingency plans, and strengthening the capacity of health systems to withstand and adapt to external shocks, such as conflicts, epidemics, and natural disasters. A resilient health system can maintain essential services and recover quickly from disruptions, ensuring continuity of care and protecting public health.
Strategic planning is crucial for guiding health systems in fragile states towards achieving their long-term goals and addressing complex health challenges. It provides a structured framework for decision-making, enhances coordination among stakeholders, and ensures the efficient use of resources, ultimately leading to improved health outcomes and greater system resilience8.
Chapter Three
Key Elements of Effective Strategic Planning in Fragile States
A. Situation Analysis and Needs Assessment
Gathering and Analyzing Data on Health Needs and System Capacities
Effective strategic planning in fragile states begins with a thorough situation analysis and needs assessment. This process involves gathering comprehensive data on the health needs of the population and the existing capacities of the health system. This includes epidemiological data, health service availability, infrastructure quality, and workforce capacity. The data collection methods may involve surveys, health information systems, and direct observations. Accurate and detailed data is crucial for understanding the health landscape, identifying gaps, and informing decision-making.
Involving Stakeholders in the Assessment Process
Stakeholder involvement is essential in the needs assessment process to ensure that the perspectives and needs of different groups are considered. This includes government agencies, healthcare providers, non-governmental organizations (NGOs), community leaders, and the affected population. Engaging stakeholders helps to build consensus, foster collaboration, and ensure that the strategic plan is relevant and feasible. It also enhances the credibility and acceptance of the plan, increasing the likelihood of successful implementation.
B. Setting Priorities and Objectives
Identifying Critical Health Issues and Setting Achievable Goals
Once the needs assessment is completed, the next step is to identify critical health issues that need to be addressed. This involves prioritizing health problems based on their severity, impact on the population, and feasibility of intervention. Setting clear, achievable goals is crucial for guiding the strategic planning process. These goals should be specific, measurable, attainable, relevant, time-bound, evaluated, and reviewed (SMARTER). Prioritization helps to focus resources and efforts on the most pressing health issues, ensuring that the interventions are impactful and sustainable.
Aligning Objectives with Available Resources and Capacities
It is important to align the objectives of the strategic plan with the available resources and capacities of the health system. This includes financial resources, human resources, infrastructure, and technological capabilities. Realistic alignment ensures that the goals are achievable and that the health system can effectively implement the planned interventions. It also helps to identify resource gaps that need to be addressed through external support or innovative solutions.
C. Resource Mobilization and Allocation
Securing Funding and Resources from International Donors and Local Sources
Resource mobilization is a critical component of strategic planning in fragile states. This involves securing funding and other resources from both international donors and local sources. International donors, including multilateral organizations, foreign governments, and global health initiatives, play a significant role in providing financial and technical support. Local sources of funding may include government budgets, private sector contributions, and community fundraising efforts. Diversifying funding sources helps to ensure financial sustainability and reduce dependency on a single source.
Efficient Allocation of Resources to Priority Areas
Effective strategic planning requires the efficient allocation of resources to priority areas. This involves distributing funds, personnel, and materials in a way that maximizes their impact on health outcomes. Resource allocation should be guided by the priorities and objectives set during the planning process, ensuring that the most critical health issues receive adequate attention. Monitoring and evaluation mechanisms are essential for tracking resource use and making necessary adjustments to improve efficiency and effectiveness.
D. Implementation and Monitoring
Developing Actionable Plans with Clear Timelines and Responsibilities
Implementation is a crucial phase of strategic planning, requiring the development of actionable plans with clear timelines and assigned responsibilities. Detailed action plans outline the specific steps needed to achieve the strategic goals, including activities, milestones, and deliverables. Clearly defined roles and responsibilities ensure accountability and facilitate coordination among different stakeholders. Action plans should be flexible to adapt to changing circumstances and emerging challenges.
Establishing Monitoring and Evaluation Frameworks to Track Progress and Outcomes
Monitoring and evaluation (M&E) frameworks are essential for tracking the progress and outcomes of the strategic plan. These frameworks include indicators, data collection methods, and reporting mechanisms to measure the performance of the interventions. Regular monitoring helps to identify issues early, allowing for timely adjustments and improvements. Evaluation provides insights into the effectiveness and impact of the strategic plan, informing future planning and decision-making processes. M&E frameworks enhance transparency and accountability, building trust among stakeholders and donors.
E. Capacity Building and Workforce Development
Training and Retaining Healthcare Workers
Capacity building and workforce development are fundamental to the success of strategic planning in fragile states. This involves training healthcare workers to improve their skills and competencies, ensuring that they can deliver high-quality services. Training programs should be continuous and cover various aspects of healthcare, including clinical skills, management, and leadership. Retaining trained healthcare workers is equally important, requiring strategies such as competitive salaries, career development opportunities, and supportive working conditions9.
Strengthening Institutional Capacities for Better Service Delivery
In addition to individual capacity building, strengthening the institutional capacities of health organizations is crucial for effective service delivery. This includes improving health governance, management systems, infrastructure, and technology. Institutional strengthening helps to create a supportive environment for healthcare workers and ensures that the health system can effectively implement and sustain the strategic plan. It also involves fostering a culture of continuous improvement and innovation within health institutions.
By addressing these key elements, strategic planning can significantly enhance health systems in fragile states, improving health outcomes and building resilience against future challenges.
But for this to be achieved, what are the foundations of health system strengthening in fragile states?
In a study done by Birke Bogale, Sasha Scambler, Aina Najwa Mohd Khairuddin, and Jennifer E. Gallagher published in PLOS ONE they found that there are five pillars to reach a robust health systems10:
1. Population
Cultural norms, community engagement, and collaboration are crucial for improving health outcomes in conflict-affected settings, especially among displaced populations in low- and middle-income countries. Overcoming cultural and religious barriers is essential for effective care, and community involvement in mental health care, healthcare worker support, and health promotion among refugees can bridge service delivery gaps. Training community members, including refugee healthcare workers, helps bridge workforce gaps, and collaboration ensures a safe environment for healthcare workers. Community-driven programs enhance healthcare delivery by involving traditional leaders and empowering community members to propose solutions.
2. Governance
Health system governance and coordination in fragile and conflict-affected settings, such as humanitarian disasters and post-conflict reconstruction, face challenges like unclear responsibilities, mistrust, financial barriers, and inadequate infrastructure. Effective governance, political commitment, and leadership are crucial for enhancing health system performance. Strategies like decentralization, community-based health insurance, performance-based financing, and coordinated donor funding are beneficial. People-centric governance, effective coordination mechanisms, and appropriate financing models are essential. Countries should own their health financing to minimize external influences and ensure long-term governance.
3. Platforms
Healthcare access and service platforms in crisis situations face challenges such as security concerns, non-functioning facilities, staff shortages, distance to facilities, and refugee influxes. The availability of medicines is also a significant issue. Various healthcare models have been used, including integrating NCD interventions into primary healthcare and using camp-based structures. Strategies to improve vaccination delivery include fixed-sites, mobile teams, and mass-vaccination sites coordinated by the Ministry of Health and NGOs. Community-based health services, mobile healthcare teams, and partnerships with private providers and traditional healers have shown benefits in improving healthcare access. Tailored and context-specific healthcare models are crucial for effective intervention planning.
4. Workforce
The study highlights the challenges faced by healthcare workers in fragile states, including safety, financial incentives, conflict, and gender barriers. High turnover rates are due to targeted attacks, displacement, and inadequate financial incentives. Conflict disrupts training and education, leading to a shortage of skilled trainers and poor-quality on-the-job training. Community support and intrinsic motivations help some workers stay or return. Recommendations include prioritizing safety, offering competitive salaries, ensuring equitable distribution, investing in standardized training programs, improving work conditions, and rebuilding infrastructure to retain staff. These measures aim to enhance healthcare services in fragile states and address workforce stability and effectiveness.
5. Tools
The lack of adequate physical resources and supervision in health systems in fragile states is a significant issue. This affects healthcare quality and worker retention. Despite the need for effective supervision, many facilities, particularly in rural areas, lack strict systems. Conflict also limits the number of capable managers and supervisors. Poor-quality and inconsistent data collection further delays health system reforms; eHealth tools, like mobile applications and telehealth, improve data management and healthcare delivery, but often lack systematic protocols. To improve healthcare services in fragile states, it is crucial to improve physical resources, implement effective supervision, and standardize eHealth interventions.
Chapter Four
Challenges in Strategic Planning for Health Systems in Fragile States
A. Political Instability and Governance Issues
Political instability and weak governance are major obstacles to strategic planning in fragile states. Frequent changes in government, political unrest, and corruption can disrupt the continuity of health policies and their implementation11. When new administrations come to power, they often prioritize different agendas, leading to shifts in health policies and strategies. This lack of continuity hampers long-term planning and the consistent execution of health initiatives. Furthermore, weak governance structures may lack the capacity to enforce policies effectively, resulting in gaps and inconsistencies in service delivery.
B. Resource Constraints
Fragile states often face severe resource constraints that limit their ability to implement strategic health plans. Financial limitations are common, with inadequate funding from both domestic budgets and international aid. These financial constraints affect the procurement of essential supplies, the maintenance of health facilities, and the payment of healthcare workers. Human resource limitations, such as shortages of trained healthcare professionals, further strain the health system. Additionally, infrastructural limitations, including inadequate health facilities and poor transportation networks, impede the delivery of health services, particularly in remote and underserved areas. Last, the lack of technical expertise such as skills in data analysis and strategic thinking can cause an important challenge to overcome12.

C. Coordination and Collaboration Difficulties
Effective strategic planning requires the coordination and collaboration of various stakeholders, including government agencies, NGOs, and international organizations. In fragile states, this coordination is often challenging due to fragmented efforts, competing priorities, and limited communication. Governments may lack the authority or capacity to lead and coordinate these efforts, leading to duplicative or conflicting interventions. Additionally, NGOs and international organizations may operate independently, without aligning their activities with national health strategies. This lack of coordination undermines the efficiency and effectiveness of health interventions and wastes valuable resources.
D. Cultural and Social Barriers
Cultural and social barriers can significantly impact the success of strategic health plans in fragile states. Cultural beliefs and practices may influence health-seeking behaviors, acceptance of medical interventions, and perceptions of health and illness. For example, traditional medicine practices may conflict with modern healthcare approaches, leading to resistance or mistrust among communities. Social determinants of health, such as poverty, education, and gender inequality, also play a critical role in health outcomes. Addressing these cultural and social barriers requires culturally sensitive approaches that respect local traditions while promoting evidence-based health practices. Engaging community leaders and stakeholders is essential to build trust and ensure the acceptance of health interventions13.
By understanding and addressing these challenges, strategic planners can develop more effective and resilient health systems in fragile states, ultimately improving health outcomes and enhancing the well-being of vulnerable populations.
Chapter Five
Strategies for Overcoming Challenges
A. Strengthening Governance and Leadership
To overcome the challenges posed by political instability, it is crucial to promote political stability and effective governance. This can be achieved through various means, including fostering inclusive political processes, strengthening democratic institutions, and combating corruption. International organizations and donor countries can support fragile states by providing technical assistance and resources to enhance governance structures. Effective governance also requires clear and consistent health policies that are insulated from political fluctuations, ensuring that strategic health plans are implemented and sustained over the long term.
Strengthening leadership capacities within health ministries is essential for effective strategic planning and implementation. Training programs and workshops can be designed to enhance the skills of health ministry officials in areas such as strategic management, policy development, and health economics. Building a cadre of competent leaders who can navigate the complexities of fragile state environments will improve decision-making, resource allocation, and the overall effectiveness of health interventions.
B. Enhancing Community Engagement and Ownership
Engaging communities in the planning and decision-making processes of health interventions is critical for ensuring their success and sustainability. Community involvement helps to tailor health initiatives to the specific needs and preferences of the population, increasing their acceptance and effectiveness. Participatory approaches, such as community consultations and focus groups, can be used to gather input and feedback from community members. This involvement fosters a sense of ownership and accountability, encouraging communities to support and sustain health interventions.
Building trust and collaboration between communities and health providers is essential for the successful implementation of health interventions. Trust can be established by involving community leaders in the planning and delivery of health services, ensuring transparency in decision-making processes, and providing culturally sensitive care. Health providers should engage with communities regularly to address their concerns and build strong relationships. Collaborative efforts can lead to better health outcomes by ensuring that services are responsive to community needs and that community members actively participate in promoting health and well-being.
C. Leveraging Technology and Innovation
Leveraging technology and innovation can significantly enhance health system performance in fragile states. Digital health tools, such as mobile health applications, telemedicine, and electronic health records, can improve access to health services, facilitate data collection, and enhance communication between health providers and patients. These tools can also support disease surveillance, monitoring, and evaluation activities, enabling timely and evidence-based decision-making. Investing in technology infrastructure and training health workers to use digital tools can help bridge gaps in service delivery and improve health outcomes.
Innovative solutions are needed to address the unique challenges of delivering health services in fragile states. Examples include community health worker programs, mobile clinics, and low-cost diagnostic tools. These innovations can extend the reach of health services to remote and underserved areas, ensuring that vulnerable populations receive the care they need. Additionally, partnerships with the private sector and non-governmental organizations can foster innovation by leveraging their expertise and resources to develop and scale up effective health solutions.
D. Fostering International Partnerships and Support
International partnerships and support are crucial for addressing the challenges of strategic planning in fragile states. Collaborating with international organizations, such as the World Health Organization (WHO), the United Nations (UN), NGOs, can provide technical assistance, funding, and resources to support health interventions. These partnerships can also facilitate knowledge sharing and capacity building, helping fragile states to develop and implement effective health strategies.
To maximize the impact of international aid, it is essential to align it with national health priorities and strategic plans. Donors and international organizations should work closely with national governments to ensure that their support addresses the most pressing health needs and strengthens the overall health system. This alignment can be achieved through joint planning and coordination mechanisms, such as health sector coordination committees and donor harmonization initiatives. By aligning aid with national priorities, international support can contribute to sustainable health system strengthening and improved health outcomes in fragile states.
In a study conducted by USAID titled “From Humanitarian and Post-conflict Assistance to Health System Strengthening in Fragile States: Clarifying the Transition and the Role of NGOs”, the phases of health interventions, the role of NGOs, transition strategies, and challenges in transition are explored14:
Phases of Health Interventions: The study identifies three critical phases. The first phase, Immediate Health Needs, focuses on addressing urgent crises through emergency humanitarian response, providing quick, life-saving interventions.
The second phase, Restoring Essential Health Services, aims to re-establish basic health services and delivery mechanisms, ensuring that essential care is available to the population.
In the third phase, Rehabilitating the Health System, the focus shifts to building long-term capacity through governance, policy-making, workforce training, and infrastructure development.
Role of NGOs: NGOs are crucial, particularly in providing immediate health services during emergencies when local government capacity is lacking. They are often contracted by donors to fill gaps in service delivery. In the longer term, NGOs assist in transitioning healthcare systems from short-term emergency responses to long-term system strengthening.

Transition Strategies: Successful transitions involve shifting from bypassing local governments to partnering with them for both service delivery and capacity building. For example, in Timor Leste (a Southeast Asian country that gained independence in 2002 following conflict), initial emergency responses by NGOs gradually transitioned to government-led health system management, ensuring long-term sustainability.
Challenges in Transition: Key include Donor Coordination, where fragmented assistance can result in inefficiency. Sustainability is another challenge, as balancing immediate response needs with long-term capacity-building efforts requires careful resource allocation. Lastly, the transition is an Iterative Process that demands flexibility and continuous adaptation to evolving circumstances.
By applying these strategies, fragile states can overcome the challenges of strategic planning and build resilient health systems capable of addressing both immediate and future healthcare needs.
Chapter Six
Future Directions
A. Emerging Trends in Health Systems Strengthening
Global health security is increasingly recognized as a critical component of health systems strengthening, especially in fragile states. This concept emphasizes the importance of protecting populations from global health threats, such as pandemics, through robust health infrastructure and international cooperation. For fragile states, global health security entails building capacity for disease surveillance, emergency response, and health system resilience. By focusing on global health security, fragile states can enhance their ability to prevent, detect, and respond to health emergencies, thereby protecting their populations and contributing to global health stability.
The integration of health and development agendas is essential for achieving sustainable improvements in health systems. Health outcomes are closely linked to social, economic, and environmental determinants, making it necessary to adopt a holistic approach to development. In fragile states, integrating health initiatives with broader development efforts can address underlying determinants of health, such as poverty, education, and infrastructure. Collaborative efforts between health and development sectors can lead to comprehensive strategies that promote overall well-being and resilience. This approach requires coordinated policies and programs that align health goals with development priorities, ensuring that health improvements are sustainable and inclusive.
B. Policy Recommendations
Policymakers in fragile states can enhance health systems by adopting several strategic planning strategies:
1. Prioritize Health System Strengthening: Recognize health system strengthening as a national priority and allocate sufficient resources to support strategic planning and implementation efforts.
2. Develop Inclusive Policies: Ensure that health policies are inclusive and consider the needs of all population groups, especially vulnerable and marginalized communities.
3. Enhance Data Systems: Invest in robust health information systems to support data-driven decision-making and monitor the impact of health interventions.
4. Promote Accountability and Transparency: Establish mechanisms for accountability and transparency in health governance to build trust and ensure efficient use of resources.
5. Strengthen Health Workforce: Focus on training, retaining, and motivating health workers to build a competent and resilient health workforce.
International donors and partners can play a significant role in supporting health systems strengthening in fragile states:
1. Align Support with National Priorities: Ensure that aid and technical assistance align with the national health priorities and strategic plans of recipient countries.
2. Foster Long-Term Partnerships: Build long-term partnerships with national governments and local organizations to ensure sustainable impact and capacity building.
3. Promote Flexibility and Adaptability: Design aid programs that are flexible and adaptable to changing contexts and emerging challenges in fragile states.
4. Support Innovation and Technology: Invest in innovative solutions and technologies that can enhance health service delivery and system resilience.
5. Encourage South-South Cooperation: Facilitate knowledge sharing and collaboration between fragile states to leverage successful experiences and best practices.
C. Long-Term Vision for Health Systems in Fragile States
The long-term vision for health systems in fragile states should focus on building sustainability and resilience. This involves creating health systems that can withstand and adapt to various shocks, including political instability, economic crises, and health emergencies. Key components of resilient health systems include strong governance, reliable funding mechanisms, a well-trained health workforce, and robust health infrastructure. Additionally, resilient health systems should be capable of continuous learning and improvement, incorporating feedback and evidence to enhance performance over time.
Equity and accessibility should be central to the long-term vision for health systems in fragile states. This means ensuring that all individuals, regardless of their socioeconomic status, geographical location, or background, have access to quality health services. Strategies to promote equity and accessibility include:
1. Expanding Coverage: Implementing policies and programs that extend health coverage to underserved and remote populations.
2. Reducing Financial Barriers: Developing financing mechanisms, such as universal health coverage (UHC) schemes, to reduce out-of-pocket expenses and financial barriers to care.
3. Addressing Social Determinants: Tackling social determinants of health, such as education, housing, and nutrition, to improve overall health outcomes.
4. Promoting Inclusive Policies: Ensuring that health policies are inclusive and consider the needs of all population groups, particularly the most vulnerable.
By focusing on these future directions, fragile states can develop robust, equitable, and resilient health systems that improve health outcomes and contribute to overall societal stability and development.
Chapter Seven
Case Studies
A. Afghanistan
Historical Context and Health System Challenges
Afghanistan has experienced decades of conflict, political instability, and socioeconomic challenges, severely impacting its health system. The prolonged war has led to the destruction of health infrastructure, displacement of populations, and a significant brain drain of healthcare professionals. The health system faces numerous challenges, including limited access to healthcare services, a high burden of communicable diseases, poor maternal and child health outcomes, and inadequate healthcare financing and resources.
Strategic Planning Initiatives and Their Impacts
Afghanistan's health system has made significant progress over the past 17 years, increasing health service coverage to reach 87% of the population within two hours of travel. In 2018, about 3,135 health facilities were operational. The National Health Policy 2015-20 focuses on governance, institutional development, public health, health services, and human resources, supported by WHO and UN agencies. Achievements include the development of a new health package for universal health coverage, the National Health Strategy 2016-20, the SEHATMANDI program (2018-21), and the establishment of various health councils and regulatory authorities. Health facilities include 986 sub-centres, 873 basic health centres, 432 comprehensive health centres, and others. However, challenges such as poverty, distance, high costs, insecurity, and a shortage of female healthcare providers hinder optimal service utilization. The way forward involves prioritizing health system development, implementing the National Health Policy, revising health service packages, and aligning with Sustainable Development Goals (SDGs) and the Afghanistan National Peace and Development Framework15.
Strategic planning initiatives in Afghanistan have focused on rebuilding the health infrastructure, improving access to essential health services, and strengthening health governance. Key strategies include:
• Basic Package of Health Services (BPHS): Introduced to provide a standardized set of essential health services at primary healthcare facilities across the country. The BPHS has improved access to healthcare, particularly in rural and underserved areas, and has contributed to better maternal and child health outcomes.
• Health Management Information System (HMIS): Implemented to enhance data collection, monitoring, and decision-making processes. The HMIS has improved the availability and use of health data, enabling more effective planning and resource allocation.
• Community Health Worker (CHW) Program: Expanded to train and deploy community health workers in remote areas. This program has increased healthcare coverage, facilitated health education, and improved disease prevention and management at the community level.
These strategic planning initiatives have led to notable improvements in health indicators, including increased immunization coverage, reduced maternal and child mortality rates, and enhanced service delivery in conflict-affected regions.
B. South Sudan
Health System Overview and Challenges
South Sudan, the world's youngest country, has faced ongoing civil conflict, political instability, and severe humanitarian crises since gaining independence in 2011. The health system is characterized by a lack of infrastructure, insufficient healthcare workforce, and inadequate funding. High levels of poverty, malnutrition, and infectious diseases further exacerbate the health challenges.
South Sudan, plagued by conflict, flooding, and the COVID-19 pandemic, faces significant health challenges, with over 8 million people requiring humanitarian assistance in 2021. The country's health indicators are poor, marked by high maternal, infant, and child mortality rates and a low life expectancy of 56.5 years. Despite these challenges, efforts are being made to transition from humanitarian relief to long-term health sector development16.
Key Initiatives and Achievements
• Global Action Plan for SDG3: This initiative involves 13 multilateral agencies, including WHO, working towards achieving health-related Sustainable Development Goals (SDGs) in South Sudan. These agencies collectively contribute about one-third of global development assistance for health.
• Identifying Priority Challenges: WHO and UNICEF supported the Ministry of Health in identifying key priorities such as strengthening leadership and governance, health commodity management, equitable service delivery, and community systems strengthening.
• Strategic Planning: In collaboration with the Ministry of Health, WHO conducted a health sector performance review in 2021, which informed the strategic plan aimed at integrating the COVID-19 recovery strategy into primary health care (PHC).
• Stakeholder Coordination: WHO revitalized the health development partners forum secretariat and co-chairs the Health Sector Steering Committee, ensuring that interventions are harmonized with national priorities.
• Action Plan Development: In 2021, the Global Action Plan Primary Healthcare (GAP PHC) accelerator working group, including WHO, developed an action plan to map financing, identify gaps, and advocate for additional resources.
• Capacity Building: WHO provided leadership and management training to 48 senior leaders, resulting in key recommendations for improving health sector governance, endorsed during the inaugural Ministerial Advisory Board meeting.
• Essential Health Services Package (EHSP): Developed to provide a comprehensive range of basic health services, including maternal and child health, immunization, and treatment of common illnesses. The EHSP has improved access to essential healthcare and reduced mortality rates among vulnerable populations.
• Health Pooled Fund (HPF): Established to coordinate donor funding and support the delivery of health services. The HPF has enhanced resource allocation, improved health infrastructure, and strengthened health governance and accountability.
• Integrated Community Case Management (ICCM): Implemented to train community health workers in diagnosing and treating common childhood illnesses. The ICCM has increased access to life-saving treatments and reduced child mortality rates in remote areas.
The challenges faced in healthcare delivery include sub-optimal utilization of services, primarily driven by poverty and geographical distance, which hinder access. Access issues are compounded by high costs, low awareness of available services, insecurity, and a shortage of female healthcare providers, which particularly affects women's health services. Additionally, there is low government funding for health initiatives, coupled with reduced donor support, which further strains resources. Resource allocation is inadequate, with domestic resources being limited and execution capacity at sub-national levels remaining low, making it difficult to effectively implement health programs.
Way Forward
WHO, alongside the Ministry of Health and partners, focuses on health system development, implementation of national health strategies, revision of health service packages, and alignment with SDGs and the Afghanistan National Peace and Development Framework. This approach aims to transition from immediate relief to sustainable health sector development, emphasizing primary health care as a pathway to universal health coverage.
By continuing to advocate for resources and building leadership capacity, WHO and its partners are committed to strengthening South Sudan's health system to improve health outcomes and resilience in the face of ongoing challenges.
Despite the ongoing challenges, these strategic interventions have contributed to improved health outcomes and increased resilience of the health system in South Sudan.
C. Lebanon
Health System in the Context of Economic and Political Instability
Lebanon's health system has been profoundly impacted by a series of economic, political, and social crises. The country has faced a severe economic collapse, political gridlock, and the burden of hosting a large number of Syrian refugees. These challenges have strained the healthcare system, leading to a significant shortage of medical supplies, a decrease in healthcare funding, and the emigration of many healthcare professionals.
The economic crisis, characterized by hyperinflation and a collapsing currency, has severely limited the government’s ability to finance healthcare. Public hospitals and healthcare centers have faced budget cuts, leading to diminished services and deteriorating infrastructure. Political instability and frequent government changes have disrupted policy continuity and the implementation of long-term health strategies. The influx of Syrian refugees has placed additional pressure on the healthcare system, necessitating increased healthcare services without corresponding increases in funding or resources.
Strategic Planning Efforts and Their Effectiveness
In response to these multifaceted challenges, Lebanon has implemented several strategic planning efforts aimed at stabilizing the health system, ensuring continuity of care, and improving health outcomes. Key strategies include:
• Lebanon Health Resilience Project (LHRP): This project who is sponsored by the World Bank aims to enhance the resilience of the Lebanese health system by improving the capacity of health facilities to respond to emergencies and crises. The LHRP focuses on strengthening primary healthcare services, which are crucial for providing accessible and cost-effective care to the population, including refugees. Through the LHRP, health centers have received support in the form of medical supplies, training for healthcare workers, and infrastructure upgrades. This initiative has been instrumental in maintaining service delivery during times of crisis and in ensuring that vulnerable populations have access to essential health services17.
• National Health Strategy 2030: This long-term strategic plan provides a comprehensive vision for the health system in Lebanon. The strategy outlines goals for improving health governance, expanding healthcare coverage, enhancing the quality of care, and promoting health equity. The strategy sets out immediate actions for relief and five strategic directions for sector recovery18:
- Strengthened Health Sector Governance: Institutionalizing collaborative governance, enhancing Ministry leadership, decentralizing and providing autonomy to public hospitals, and ensuring health security and public health functions.
- Financial Protection and Universal Health Coverage: Addressing health financing fragmentation, promoting public-private partnerships, and ensuring financial risk protection.
- Health Service Delivery: Enhancing primary health care, private ambulatory care, and addressing outpatient and inpatient care.
- Health Security and Disease Prevention: Strengthening preparedness and response to disease outbreaks and natural disasters.
- Health Workforce and Health Information System: Improving the health workforce's capacity and enhancing health information systems.
• E-Health Initiatives: Leveraging digital technology to improve health information systems, enhance telemedicine services, and provide digital health solutions. These initiatives aim to increase the efficiency and reach of healthcare services, especially in remote and underserved areas. E-health platforms facilitate better patient management, remote consultations, and efficient data sharing among healthcare providers. These technologies have been particularly useful during the COVID-19 pandemic, enabling continued access to healthcare while minimizing physical contact.
• Public-Private Partnerships: The Lebanese health system has increasingly relied on collaborations between the public sector and private entities to enhance service delivery and resource mobilization. These partnerships have allowed for shared investments in health infrastructure, improved access to advanced medical technologies, and better management of health services. Private sector involvement has also been crucial in filling gaps left by the public sector due to budget constraints.
• Health Equity Initiatives: Focused on ensuring that all segments of the population, including refugees and marginalized groups, have access to quality healthcare services. Programs have been implemented to provide subsidized healthcare, improve maternal and child health, and address non-communicable diseases. Community outreach and health education campaigns have also been essential components of these initiatives, raising awareness about health issues and promoting preventive care.
Effectiveness of Strategic Planning Efforts
The strategic planning efforts in Lebanon have shown positive impacts despite the challenging environment. Key achievements include:
• Improved Access to Healthcare: The expansion of primary healthcare services and the introduction of telemedicine have increased access to healthcare for both Lebanese citizens and refugees. This has been crucial in maintaining public health during times of economic and social turmoil.
• Enhanced Health System Resilience: Investments in health infrastructure and capacity building have strengthened the system's ability to respond to emergencies, such as the COVID-19 pandemic and the Beirut port explosion. The LHRP has been particularly effective in ensuring that health facilities can continue operating under adverse conditions.
• Better Resource Allocation: Strategic planning has facilitated more efficient use of limited resources, ensuring that critical areas such as maternal and child health, infectious diseases, and non-communicable diseases receive the necessary attention and funding.
• Increased Collaboration: Public-private partnerships and international donor support have provided much-needed resources and expertise, contributing to the stabilization and improvement of health services.
However, the ongoing economic crisis continues to pose significant obstacles to achieving sustainable health outcomes. The frequent changes in government, corruption, and financial constraints make it challenging to implement long-term strategies effectively. Despite these challenges, the strategic planning efforts in Lebanon demonstrate the importance of coordinated and well-planned initiatives in maintaining and improving health systems in fragile contexts.
Conclusion
Strategic planning is crucial in enhancing health systems in fragile states. These states face unique challenges, such as political instability, economic hardships, and limited resources, which impede the delivery of effective healthcare services. Strategic planning provides a structured approach to addressing these challenges by setting clear goals, allocating resources efficiently, and implementing evidence-based interventions. By fostering coordination among stakeholders, improving resource allocation, and building system resilience, strategic planning can lead to significant improvements in health outcomes in fragile contexts. Case studies from Afghanistan, South Sudan, and Lebanon illustrate how strategic planning initiatives have positively impacted health systems, demonstrating its critical role in these environments.
Prioritizing inclusive and data-driven planning ensures that strategic plans address the specific health needs of diverse population groups. Strengthening stakeholder collaboration is essential for aligning efforts and leveraging resources effectively among government agencies, non-governmental organizations, international donors, and local communities. Investing in capacity building focuses on training and retaining healthcare workers, strengthening institutional capacities, and building robust health information systems to support sustainable improvements. Encouraging the adoption of innovative solutions and technologies, such as telemedicine and mobile health units, can enhance healthcare delivery in challenging environments. Implementing mechanisms for accountability and transparency in health governance builds trust and ensures efficient use of resources. Developing strategies for resource mobilization and efficient allocation ensures that funding is aligned with national health priorities and strategic plans.
The dynamic and often volatile nature of fragile states necessitates ongoing strategic planning to address the complex challenges facing their health systems. While strategic planning has proven effective in enhancing health systems, it is not a one-time solution. Continuous assessment, adaptation, and improvement of strategies are essential to respond to evolving needs and emerging threats. The commitment of national governments, supported by international partners, to sustained strategic planning and implementation efforts is crucial for building resilient, equitable, and sustainable health systems. By prioritizing strategic planning, fragile states can make significant strides towards achieving better health outcomes and overall societal stability, contributing to global health security and development.

Note: As this article is being finalized, Lebanon is facing a new crisis due to recent Israeli aggression, which has resulted in more than 10,000 wounded individuals so far. This situation has placed additional strain on an already fragile healthcare system, exacerbating the challenges discussed in this article. The ongoing conflict highlights the urgent need for robust and adaptable strategic planning to ensure that healthcare systems in fragile states like Lebanon can respond effectively to both chronic structural weaknesses and acute emergencies.
References
1. Birke Bogale, Sasha Scambler, Aina Najwa Mohd Khairuddin, Jennifer E. Gallagher, Health system strengthening in fragile and conflict-affected states: A review of systematic reviews, PLOS ONE, June 14,2024.
2. Derick W. Brinkerhof (2008) From Humanitarian and Post-conflict Assistance to Health System Strengthening in Fragile States: Clarifying the Transition and the Role of NGOs, USAID.
3. Rohini J. Haar & Leonard S. Rubenstein (2012) Health in fragile and postconflict states: a review of current understanding and challenges ahead.
4. Lebanon National Health Strategy: Vision 2030.
5. World Health Organization, Health System Strengthening, Afghanistan.
6. Strengthening primary health care in fragile settings: South Sudan, World Health Organization.
7. Fragile States Index, available on https://fragilestatesindex.org
8. The University of Arizona Global Campus, What is Strategic Planning in Health Care?, 18 december 2024, available on https://www.uagc.edu/blog/what-strategic-planning-health-care
9. Hu, Q., Kapucu, N., & O'Byrne, L. (2014). Strategic planning for community-based small nonprofit organizations: Implementation, benefits, and challenges. The Journal of Applied Management and Entrepreneurship.
10. OECD. (2018). States of Fragility 2018. OECD Publishing.
11. World Health Organization. (2020). Health systems in conflict-affected fragile settings. WHO.
12. Collier, P., & Hoeffler, A. (2004). Greed and grievance in civil war. Oxford Economic Papers.
13. Kruk, M. E., Ling, E. J., Bitton, A., Cammett, M., & Powers, G. F. (2017). Building resilient health systems: A proposal for a resilience index. BMJ, 357, j2323.
14. Pavignani, E., Colombo, S., & Riccardo, F. (2013). Health-service delivery in fragile states: Practical insights from experience sharing. London School of Hygiene & Tropical Medicine.
15. Global Health Cluster. (2017). Health system strengthening in fragile settings: A framework for analysis and action. World Health Organization.
16. World Bank Group, Lebanon Health Resilience Project, available on https://projects.worldbank.org/en/projects-operations/ project-detail/P163476
دور التخطيط الاستراتيجي في تعزيز الأنظمة الصحية في الدول الهشة
المقدم الصيدلي حبيب عبدو
يُعد التخطيط الاستراتيجي أداة أساسية لتعزيز النظم الصحية في الدول الهشة، التي تواجه تحديات كبرى بسبب ضعف الحوكمة، عدم الاستقرار السياسي ونقص الموارد. تعاني هذه الدول من عدم قدرتها على تقديم خدمات صحية متكاملة نتيجة للصراعات الداخلية، الفساد وتدهور البنية التحتية، ما يؤدي إلى تفاقم المشكلات الصحية وانتشار الأوبئة. إن ضعف التنسيق بين الجهات الفاعلة، بما في ذلك الحكومات والمنظمات غير الحكومية والجهات المانحة، يؤدي إلى جهود غير منظمة وهدر للموارد، ما يزيد من هشاشة النظام الصحي.
يسهم التخطيط الاستراتيجي في معالجة هذه التحديات عبر وضع أهداف واضحة، وتخصيص الموارد بشكلٍ أكثر كفاءة، وتعزيز القدرة على التكيف مع الأزمات. من خلال تحديد الأولويات الصحية بناء على تقييم دقيق للاحتياجات، يمكن تحسين توزيع الموارد وتوجيهها نحو القطاعات الأكثر احتياجًا. كما يساعد في بناء نظم صحية أكثر استدامة من خلال الاستثمار في البنية التحتية، تحسين آليات الحوكمة وتعزيز قدرات الكوادر الطبية. تضمن عمليات التقييم والمتابعة المستمرة تنفيذ الاستراتيجيات بفعاليةٍ وإجراء التعديلات اللازمة لمواكبة التغيرات.
هناك تحديات كبيرة أمام تطبيق التخطيط الاستراتيجي في هذه البيئات. فعدم الاستقرار السياسي يعوق استمرارية تنفيذ الاستراتيجيات الصحية طويلة الأمد، كما أن نقص التمويل يشكل عقبة رئيسة أمام تطوير الخدمات الصحية وتحسينها. ويؤدي ضعف التنسيق بين مختلف الفاعلين إلى تداخل الجهود وعدم الاستفادة المثلى من الموارد المتاحة. العوامل الثقافية والاجتماعية مثل الأعراف والتقاليد، قد تعرقل قبول بعض التدخلات الصحية، ما يستدعي اتباع استراتيجيات تتناسب مع السياقات المحلية.
تظهر أمثلة مختلفة من عدة دول هشة كيف ساهم التخطيط الاستراتيجي في تحسين الخدمات الصحية على الرغم من التحديات. ففي أفغانستان، ساعد تطبيق «حزمة الخدمات الصحية الأساسية» في توسيع نطاق الرعاية الصحية في المناطق الريفية، وتحسين معدلات الوفيات بين الأمهات والأطفال. وفي جنوب السودان، أدى تعزيز الشراكات الدولية إلى تحسين تقديم الخدمات الصحية، لا سيما من خلال برامج الرعاية الأولية. أما في لبنان، فقد ساعدت استراتيجيات مثل «تعزيز صمود النظام الصحي اللبناني» في مواجهة الأزمة الاقتصادية والسياسية عبر تطوير آليات جديدة لتحسين استدامة الرعاية الصحية.
تتطلب التوجهات المستقبلية تعزيز الأمن الصحي من خلال بناء نظم قادرة على الاستجابة للأوبئة والطوارئ، ودمج الصحة ضمن استراتيجيات التنمية الوطنية لضمان استدامة التقدم المحرز. يمكن أن يسهم استخدام التكنولوجيا والابتكار، مثل الطب عن بُعد وأنظمة المعلومات الصحية الرقمية، في تحسين الخدمات في المناطق النائية. إن تعزيز الشراكات بين الحكومات والمنظمات الدولية ضروري لضمان استمرارية الدعم المالي والتقني للنظم الصحية في البيئات الهشة. ويتطلب تحقيق هذه الأهداف التزامًا حكوميًا، دعمًا دوليًا مستدامًا، ونهجًا قائمًا على البيانات لضمان تحسين فعالية الأنظمة الصحية واستدامتها.